INNOVATIVE STRATEGIES IN 2025: HOW CUTTING-EDGE LABS ARE TURNING THE TIDE AGAINST ANTIMICROBIAL RESISTANT PATHOGENS
MEDICAL SCIENCE
Olaoluwa Olanusi
11/30/20254 min read
Introduction
1.2 million lives lost in 2019. 39 million projected by 2050.Antimicrobial resistance (AMR) is no longer an emerging threat it is a global crisis. Yet, in 2025, the laboratory is mounting a decisive response. This isn’t a distant nightmare. It’s happening right now in hospitals, farms, and homes across the planet.
Antimicrobial resistance isn’t “coming.” It’s here. And in 2025, for the first time in decades, the labs are finally fighting back with weapons the bacteria have never seen.
This report surveys the 2025 AMR pipeline showcases transformative platform technologies, and delivers evidence-based prevention strategies to curb the tide.
Understanding AMR: A Silent Pandemic
Antimicrobials encompass antibiotics, antivirals, antifungals, and antiparasitic essential agents for treating infections across humans, animals, and agriculture.
Antimicrobial resistance (AMR) emerges when pathogens evolve to withstand these medicines, rendering standard treatments ineffective and escalating risks of prolonged illness, disability, and mortality. Every time we use an antimicrobial – whether penicillin in a hospital or tetracycline sprinkled on chicken feed – we’re running a global Darwinian tournament. The tiny percentage of microbes that survive pass on their winning genes. Do it often enough, carelessly enough, and you breed superbugs that laugh at every drug we have.
That’s why a simple skin infection can now kill, why routine surgeries are getting riskier, and why doctors sometimes have to tell families, “There’s nothing left that works.
Primary Drivers of Resistance
1. Over-prescription – up to 50% of antibiotic scripts in humans are unnecessary (mostly for viral infections like colds).
2. Patients stopping treatment early the moment they feel better – leaving the toughest bacteria alive.
3. Self-medication and fake or under-dosed drugs in many parts of the world.
4. Agriculture – in some countries, 70–80% of all antibiotics are fed to livestock, often just to make them grow faster, not to treat disease.
The 2025 Pipeline: 90 Candidates in Development
Pathogen Class Candidates Highlights
Bacteria 80 MRSA,*Acinetobacterbaumannii
Fungi 6 Candida auris
Viruses 0 Emerging nano siRNA platforms
Context: only four truly new antibiotic classes reached patients between 2000 and 2024. Ninety in the pipe at once is unprecedented
Notable trend:44% of candidates bypass traditional antibiotics, leveraging bacteriophages, AI-designed peptides, and nanoparticle systems.
Platform Innovations Transforming Therapy
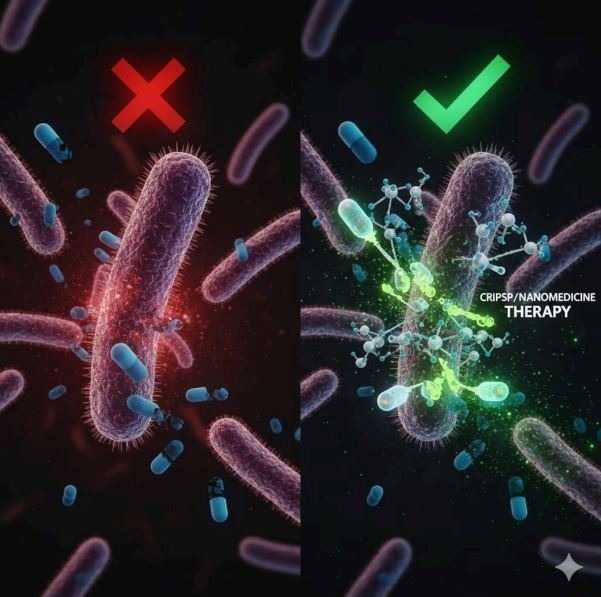
Nanoparticles: Tiny Trojan Horses That Blow Bacteria Up from the Inside
Imagine metal spheres a thousand times smaller than a red blood cell.
Iron-oxide nanoparticles stick to bacteria like magnets, rip holes in their membranes, then get recycled by your body exactly like dietary iron.
Gold nanoparticles can be studded with antimicrobial peptides – short proteins that act like heat-seeking missiles for superbugs.
Mesoporous silica nanoparticles are basically programmable drug cages that open only inside acidic biofilms (the slimy fortresses bacteria hide in).
Result: drugs reach places old antibiotics never could, with far fewer side effects.
C. CRISPR-Cas9: Precision Resistance Reversa
Target: mecA gene in MRSA (encodes PBP2a)
Action: Cleaves or silences resistance locus, (scientists are using molecular scissors to snip out the exact snippet of DNA that makes MRSA laugh at penicillin, instantly making old cheap antibiotics work again).
Result: Restores susceptibility to beta-lactam antibiotics
D. Bacteriophage Therapy
Principle: Viruses that selectively infect and lyse bacterial hosts , Phages are nature’s original antibiotics – viruses that infect only one bacterial species, inject their DNA, and explode the cell from within. After decades on the sidelines (mostly used in Georgia and Russia), Western regulators are finally fast-tracking phage therapy. Compassionate-use cases in the US and Europe are exploding, and randomized trials are launching everywhere.
Specificity: One phage, one pathogen
Status: Expanding compassionate use; clinical trials acceleration
Emerging Threats: Fungal and Viral Resistance
Candida auris
Profile: Multidrug-resistant yeast; high mortality in immunocompromised patients, auris kills up to 60% of patients who get it in their blood and can live on hospital surfaces for weeks
Challenges: Heteroresistance, robust biofilm formation
Innovation: Rezafungin analogs
Inhibit 1,3-β-glucan synthase
40% lower MIC vs. resistant isolates
Extended half-life supports weekly dosing (CDC AR Threats Report, 2025)
HIV Drug Resistance
HIV mutates faster than almost anything else alive. New countermeasure: nanoparticles carrying siRNA that silence both the virus and the human genes it hijacks – potentially turning HIV into a manageable chronic condition again with far fewer pills
Actionable Prevention Frame work
1. Seek professional diagnosis before initiating antimicrobials
2. Complete the full prescribed course even after symptom resolution
3. Avoid antibiotics for viral illnesses (e.g., influenza, common cold)
4. Practice rigorous hand hygiene to interrupt transmission
5. Next time you’re at the doctor, ask: “Do I really need this antibiotic?”
The Tool You Can Deploy Tomorrow (For Free): WHONET My Core Service in 2025
The futuristic stuff is exciting, but most hospitals need help today. That’s why WHONET has become the backbone of everything I now offer.
WHONET is the free, WHO-backed software used by over 2,500 laboratories in 130 countries to track resistance in real time. Think of it as “Google Analytics for superbugs”: you feed in daily lab results, and it instantly tells you:
Which antibiotics still work in your hospital
Which wards have rising resistance
Early outbreak alerts before they explode
Beautiful antibiograms for your stewardship committee
Want to get your lab’s first WHONET report for free? Drop me a mail at info@olanusi.com
Conclusion: From Crisis to Control
The AMR trajectory is daunting but 2025 marks a turning point
With 90 pipeline candidates, 44% non-antibiotic, and platforms like AI, CRISPR, phages, and nanoparticles converging, we are transitioning from reactive defense to proactive precision
The tools exist. The data is clear.
Now, collective action in clinical, agricultural, and individual will determine whether we contain the threat.
Share this post if you think it’s time we all got serious about saving antibiotics – before we run out of them completely.
